Postpartum Hair Loss and Everything New Moms Should Know About It
Noticing more hair shedding after childbirth can be startling, especially when it feels like one more unexpected change in an already transformative time. Yet, this phase, known as postpartum telogen effluvium, is a common and temporary response to hormonal shifts after pregnancy.
As estrogen levels decline and the body recalibrates, more hairs enter the shedding phase, creating the impression of sudden loss. Understanding why this happens can help new mothers support healthy regrowth during recovery.
At Roots by Genetic Arts (Roots by GA), we emphasize that postpartum hair loss is normal, temporary, and fully reversible. One thing new mothers may find comforting is that the process reflects a biological reset rather than permanent damage. Understanding the underlying science allows for informed recovery strategies and helps identify when a personalized approach may be needed.
-
- What Is Postpartum Hair Loss?
- Additional Factors That Can Contribute to Postpartum Hair Loss
- Simple Steps to Support Hair and Scalp Health After Childbirth
-
When to Seek Professional Help: Roots by GA’s Personalized Approach
- Why One-Size-Fits-All Treatments Don’t Always Work Postpartum
- The Bottom Line
- FAQs
What Is Postpartum Hair Loss?
The postpartum hair loss represents a temporary shift in the hair growth cycle. During pregnancy, elevated estrogen levels keep most hair follicles in the anagen (growth) phase, resulting in thicker, fuller hair. After delivery, estrogen and progesterone levels drop sharply, triggering many follicles to enter the telogen (resting) phase simultaneously.
Several months later, these resting hairs begin to shed, often in noticeable amounts1. The follicles remain active and capable of regrowth once hormonal balance is restored.
At Roots by Genetic Arts (Roots by GA), we emphasize that postpartum hair loss is normal, temporary, and fully reversible. One thing new mothers may find comforting is that the process reflects a biological reset rather than permanent damage. Understanding the underlying science allows for informed recovery strategies and helps identify when a personalized approach may be needed.
Typical Postpartum Hair Shedding Timeline
-
2–4 months after delivery:
Shedding begins as hormone levels stabilize. Increased hair fall may become visible during brushing or washing.
-
3–6 months:
Hair fall typically peaks. While this stage may appear severe, it reflects a predictable part of the cycle.
-
6–12 months:
Shedding gradually slows as follicles re-enter the growth phase.
Most individuals experience visible recovery by the first postpartum year. If thinning persists beyond 12 months or the scalp becomes increasingly visible, secondary factors such as iron deficiency, thyroid imbalance, or genetic predisposition may be contributing, warranting professional evaluation and a customized treatment plan. Early assessment and tailored care can help restore confidence and support lasting hair health beyond the postpartum phase.
Postpartum Hair Loss and Underlying Hair Disorders: A Clinical Study
A study examining 200 women with postpartum hair shedding uncovered something surprising; in most cases, it wasn’t just post-baby shedding. Only about 9.5% had pure postpartum telogen effluvium (TE), the temporary kind linked to hormonal changes. Over half (56%) actually had TE combined with androgenetic alopecia (AGA), a genetic form of hair thinning. About 6.5% had TE in addition to traction alopecia (TA) from tight hairstyles. Even more striking, 28% showed signs of all three conditions simultaneously.
In simple terms, if your hair doesn’t seem to bounce back months after delivery, it might not just be “normal shedding.” What this means is that postpartum shedding often unmasks pre-existing hair conditions such as AGA or TA that might have gone unnoticed before pregnancy. Getting an accurate diagnosis helps distinguish temporary TE from early-onset AGA, and that distinction matters 2.
The key is understanding what’s really driving your hair loss. The personalized treatment that examines your hormones, genetics, and lifestyle gives you a far better shot at full recovery than a one-size-fits-all approach. Recognizing the real cause early can make the difference between short-term shedding and long-term thinning.
| Parameter | Finding / Percentage | Description |
|---|---|---|
| Total participants | 200 | Female patients experiencing postpartum hair loss |
| Diagnosis distribution | ||
| Telogen Effluvium (TE) only | 9.5% | Patients diagnosed with TE |
| TE + Androgenetic Alopecia (AGA) | 56.0% | Patients diagnosed with both TE and AGA |
| TE + Traction Alopecia (TA)** | 6.5% | Patients diagnosed with both TE and TA |
| TE + AGA + TA** | 28.0% | Patients diagnosed with all three conditions |
| Dermoscopic findings – TE group (central scalp) | ||
| Upright regrowing hair | 100% | Observed in all TE-only patients |
| Single pilosebaceous unit | 94.7% | Observed in most TE-only patients |
| Dermoscopic findings – TE + AGA group | ||
| Upright regrowing hair | (present) | Qualitatively described, percentage not specified |
| Single pilosebaceous unit | (present) | Similar to the TE group |
| Hair diameter diversity (>20%) | >20% variation | Key diagnostic indicator of AGA involvement |
| Dermoscopic findings – TE + TA group | (similar to TE group) | No major difference reported |
| Dermoscopic findings – TE + AGA + TA group | (similar to TE + AGA group) | No difference in traction area compared to TE + TA |
| Common trichoscopic features across groups | N/A | Hair diameter diversity, empty follicles, vellus hair |
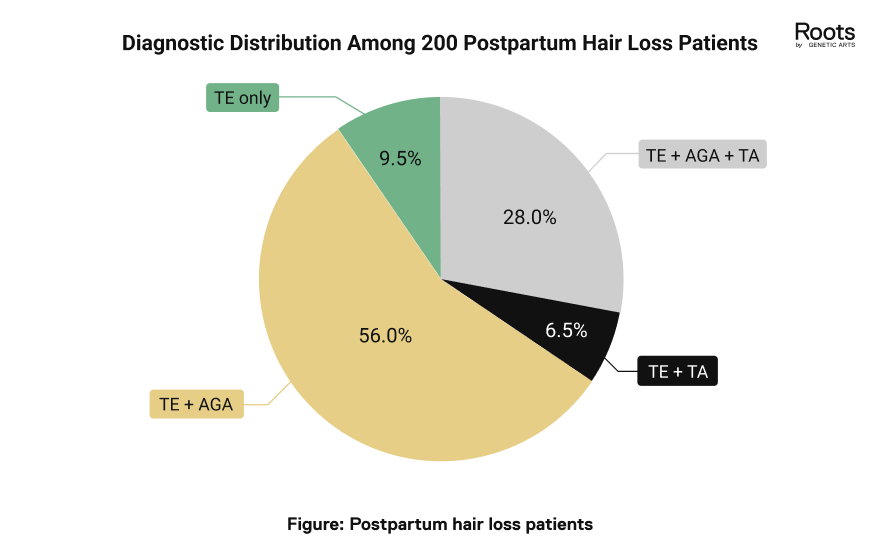
The pie chart illustrates the diagnostic distribution among 200 postpartum hair loss patients in the study. It visually highlights that the majority (56%) were diagnosed with Telogen Effluvium (TE) combined with Androgenetic Alopecia (AGA), followed by TE + AGA + TA (28%), while isolated TE and TE + TA were less common 2.
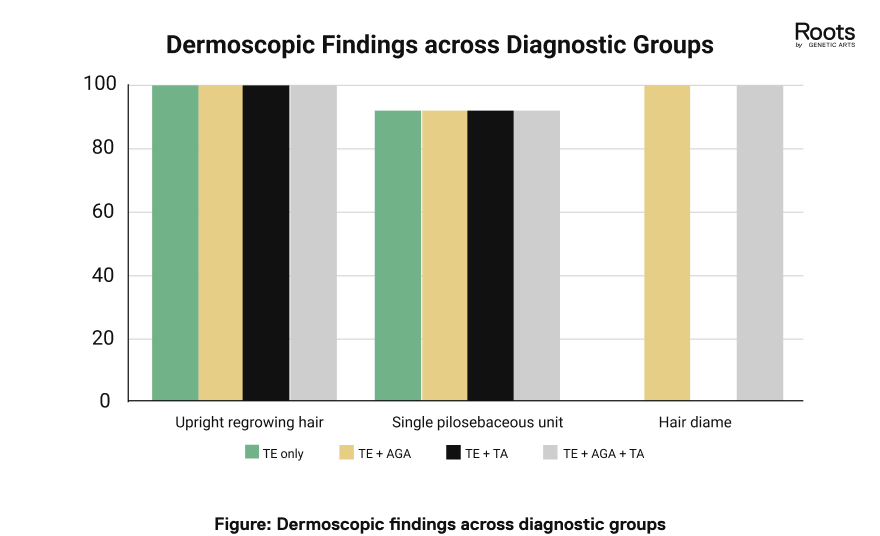
The bar chart compares dermoscopic findings across diagnostic groups. It shows that upright regrowing hair and single pilosebaceous units were nearly universal across all patient groups, whereas hair diameter diversity greater than 20% was observed only in cases involving Androgenetic Alopecia (AGA), specifically, the TE + AGA and TE + AGA + TA groups 2.
Healthy, resilient hair starts with understanding what your body truly needs.
Begin Your Personalized JourneyUse code HAIRTODAY for 30% off

Additional Factors That Can Contribute to Postpartum Hair Loss
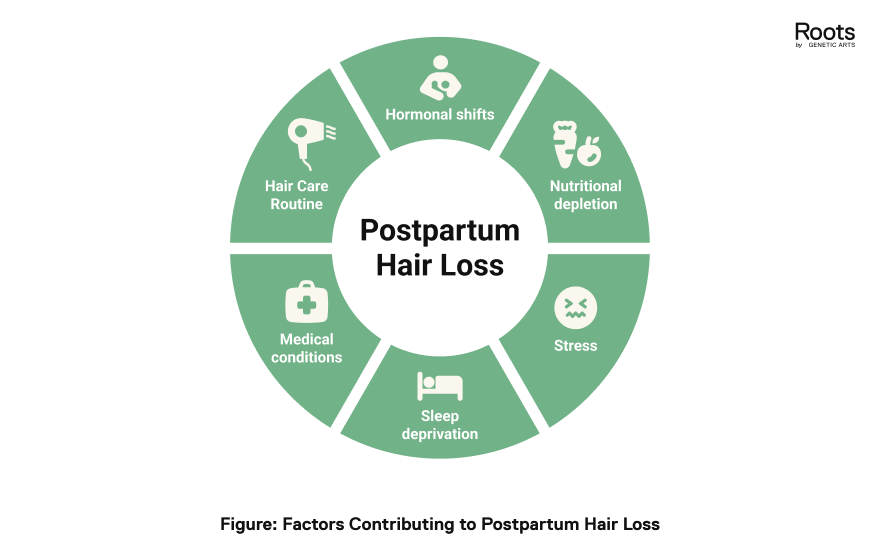
Postpartum hair shedding is often multifactorial, extending beyond hormonal changes alone. Nutritional depletion, elevated stress, sleep disturbances, and underlying medical conditions can all influence the hair growth cycle. Recognizing these contributing factors helps manage expectations and support healthy regrowth after childbirth.
Hormonal Shifts
The decline in estrogen and progesterone is accompanied by changes in prolactin and cortisol. Prolactin, essential for milk production, can delay follicle recovery, while sustained cortisol elevations from stress may accelerate shedding 3.
Nutritional Depletion
Pregnancy and breastfeeding draw heavily on nutrients vital for hair growth, including iron, zinc, vitamin D, biotin, and protein. Even mild deficiencies may trigger or intensify telogen effluvium. Clinical studies link low ferritin (iron storage) and vitamin D levels with diffuse postpartum shedding 4.
Nourish From Within
A nutrient-dense diet lays the foundation for strong follicles and balanced growth cycles.
-
Protein:
Hair consists primarily of keratin, a protein that supports follicle structure. Include lean meats, dairy, eggs, lentils, and legumes.
-
Iron and Zinc:
Essential for oxygen transport and follicle metabolism. Combine plant-based sources like lentils and spinach with vitamin C for improved absorption 4.
-
Vitamin D and Omega-3s:
Aid in regulating the hair cycle and reducing inflammation. Fatty fish, fortified foods, or flaxseed oil support these needs 4.
-
Hydration:
Adequate water intake improves circulation and nutrient delivery to follicles.
When dietary intake is insufficient, medical professionals may recommend supplements containing biotin, vitamin D, or iron. All supplementation should be supervised by a qualified clinician, particularly during breastfeeding.
Follow a Gentle Hair Care Routine
A calm and consistent approach helps minimize breakage and protect fragile strands.
-
Use mild, sulfate-free shampoos and lightweight conditioners.
-
Avoid tight hairstyles, vigorous brushing, or heat styling.
-
Massage the scalp gently for five minutes daily to enhance circulation.
-
Choose wide-tooth combs and soft microfiber towels to reduce friction.
Pro Tip
Hair follicles respond to internal equilibrium; therefore, emotional stability and physiological recovery progress in parallel. A calm internal state fosters an optimal setting for regrowth.